Iñaki Permanyer, Jordi Gumà-Lao, Sergi Trias-Llimós and Aïda Solé-Auró

Multimorbidity – where someone has two or more chronic health conditions at the same time – is a growing challenge facing health care systems, particularly in countries with low mortality rates. Although much is known about multimorbidity, important questions remain unanswered. Is it occurring more often just because people are living longer? What are the patterns of disease onset across different generations? Are some generations getting multiple chronic diseases more rapidly than others?
In an increasingly long-lived population, it’s essential for anticipating future pressures on health systems to assess whether improvements in survival prospects are accompanied by declines in illness, or whether these gains in longevity are coming at the cost of more disease and infirmity and greater care needs.
In our study recently published in the International Journal of Epidemiology, we assessed the pace at which people of different generations developed multimorbidity in Catalonia – a region in northeastern Spain with one of the highest life expectancies in the world. We looked at groups of Catalan people born in different decades and the rates at which they developed multimorbidity between 2010 and 2021.
The data used in our study come from the HEALIN cohort, a large representative population sample from the Catalan Department of Health, which has collected information on general practitioner diagnoses for more than 1.5 million people (over 20% of the entire population of Catalonia) since 2005.
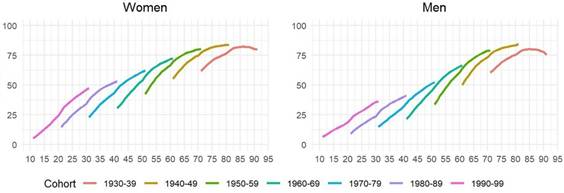
We found that younger generations tended to develop more chronic conditions than their predecessors did at the same age. For instance, by age 25, a quarter of Catalan women born between 1980 and 1989 had been diagnosed with at least two chronic conditions, whereas at the same age this was true for 37% of women born a decade later (between 1990 and 1999). This pattern was consistent across all ages and birth cohorts (see figure below), indicating an overall shift toward earlier development of multiple chronic conditions in younger generations. We also found that while people in the older cohorts were mostly affected by degenerative or other physical diseases, those from younger generations were more likely to experience mental health problems.
This pattern has also been seen in other countries, like the United States, the United Kingdom and European countries. It has been referred to as the “generational health drift” and is a matter of concern for modern-day societies that hope to achieve healthy longevity. However, little is known about the social and biological factors that may be preventing younger age groups from reaching their health potential.
There are several possible reasons for this pattern. On one hand, health outcomes might be getting worse for some population subgroups, like migrants or people of low socioeconomic status. Indeed, we found that people with low incomes have higher rates of multimorbidity than those with higher incomes. On the other hand, doctors might be tending towards overdiagnosis, possibly fuelled by technological advances, like imaging techniques. Health-seeking behaviour might also have changed over time, making people more likely to see a doctor when they are having early or only mild symptoms.
Whatever the causes, this generational health drift suggests that demands on public health care may increase, especially among younger generations. Understanding the risk factors for greater accumulation of diseases should be a focus of research, to help find effective strategies to delay or prevent multimorbidity and to slow its progression towards more severe stages and death.
Read more:
Permanyer I, Gumà J, Trias-Llimós S, Solé-Auró A. Multimorbidity trends in Catalonia, 2010-2021: a population-based cohort study. Int J Epidemiol 2026; 55: dyaf218. doi: 10.1093/ije/dyaf218.
Acknowledgement
This work was supported by the European Research Council (ERC) in relation to the research program ‘Healthy lifespan inequality: measurement, trends and determinants’, under grant no. 864616, and the Spanish Ministry of Science and Innovation R+D LONGHEALTH project (grant PID2021-128892OB-I00).
Iñaki Permanyer is an ICREA Research Professor at the Centre for Demographic Studies (CED) in the Autonomous University of Barcelona. He is Head of the Health and Aging Unit at CED and the PI of HEALIN, an ERC Consolidator Grant project (2020–2025). His research focuses on the study of population health metrics and health inequalities.
Jordi Gumà-Lao is a Ramón y Cajal Fellow at CED in the Autonomous University of Barcelona. His research is grounded in the fields of sociology of health and population studies, with a focus on gender perspectives.
Sergi Trias-Llimós is a Ramón y Cajal Fellow and Tenure-Track Assistant Professor in the Department of Political and Social Sciences at Universitat Pompeu Fabra (Barcelona). His research focuses on population health, with emphasis on inequalities in lifestyle-related health outcomes and on underlying and multiple causes of death.
Aïda Solé-Auró is an Associate Professor in the Department of Political and Social Sciences at Universitat Pompeu Fabra and a member of the DemoSoc research group. Her research sits at the intersection of demographic change and health inequality, with a focus on understanding the consequences of these dynamics for individuals’ wellbeing.
